FEB 2021, Issue 18, Vol 2
Overview
- 2021 ACA Deadlines
- Delaware Anti-Sexual Harassment Law Training Requirements
- Post OSHA 300A by February 1st
- Time to Update Your AAP’s
- Extension of FFCRA Tax Credits, Not Leave Mandate
- COVID-19 Grief Is Different: What Managers Should Know
2021 ACA Deadlines
Employers should keep in mind approaching 2021 deadlines for distributing health care reporting forms to employees and filing these forms with the IRS, as required under the Affordable Care Act (ACA).The critical filing deadlines for 2020 coverage are shown below and employers that file 250 or more information returns with the IRS must file the returns electronically.
- 1095 forms delivered to Employees - Jan. 31, 2021 (extended to 3/2/21)
- Paper filing with IRS -Feb. 28 2021
- Electronic filing with IRS - Mar. 31, 2021
- - - -
Delaware Anti-Sexual Harassment Law Training Requirements
The Delaware law that specifically addresses prohibition against sexual harassment under the Delaware Discrimination in Employment Act (DDEA), requires anti-sexual harassment training requirements for employers, with 50 or more employees in the state, every two years. The law went into effect on January 1, 2019 and in January 2021 it will be time to conduct the mandatory interactive training again.
*The law mandates all new employees must be trained within one year of hire and all employees every two years.*
Mandatory Sexual Harassment Training Required: The training for staff must include all of the following elements:
- The illegality of sexual harassment;
- The definition of sexual harassment using examples;
- The legal remedies and complaint process available to the employee;
- Directions on how to contact the Department of Labor; and
- The legal prohibition against retaliation.
In addition, the interactive training for the supervisors must further include all of the following:
- The specific responsibilities of a supervisor regarding the prevention and correction of sexual harassment; and
- The legal prohibition against retaliation.
HR Strategies, LLC is available to present interactive training programs consistent with Delaware’s training requirements. We can provide the training in-person or virtually. Contact HR Strategies to schedule your organization’s required training or schedule individual employees for a live upcoming virtual interactive class.
- - - -
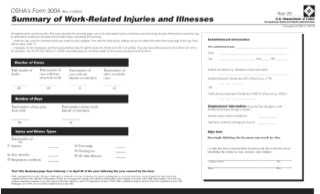
Post OSHA 300A by February 1st
Covered employers must complete and post their 2019 annual summary of work-related injuries and illnesses by February 1, 2021, and keep it posted in a common area until April 30, 2021. All employers required to keep Form 300, the Injury and Illness Log, must utilize the annual summary Form 300A to comply with posting requirements even if there have been no recordable injuries or illnesses, as the Occupational Safety and Health Administration (OSHA) will continue to focus on record-keeping violations in 2021. This year’s summary must include the total number of job-related injuries and illnesses, including COVID-19 (see later article) that occurred in 2020.
The summary Form 300A reports a business’s total year-end number of fatalities, missed workdays due to injury or illness on the job, job transfers or restrictions, and injuries and illnesses as recorded on Form 300. It also includes the number of employees and the hours they worked for the year.
Please visit www.hrstrategies.org to download the instructions and applicable forms.
- - - -
Time to Update Your AAP’s
Many Affirmative Action Plans (AAPs) expired on December 31, 2020. Under federal law, government contractors and subcontractors with 50 or more employees who have entered into at least one contract of $50,000 or more with the federal government must prepare and maintain a written affirmative action program, which must be developed within 120 days from the commencement of the contract and must be updated annually.
AAP’s should be submitted to DOL during the first quarter of 2021.
The regulations that updated Section 503 of the Rehabilitation Act of 1973 took effect on March 24, 2014. These updates required federal contractors and subcontractors to invite their employees to voluntarily self-identify their status as an individual with a disability using the Office of Federal Contract Compliance Programs’ (OFCCP) official invitation, Form CC-305 and require that contractors resurvey their workforces at least once every five years, as well as issue at least one reminder between invitations.
- - - -
Extension of FFCRA Tax Credits, Not Leave Mandate
FFCRA emergency sick leave and expanded FMLA leave mandates expired on December 31, 2020. However, covered private sector employers that allow employees to take leave that would have been mandated by the FFCRA if the law had remained in effect through March 31, 2021 may continue to claim a tax credit to cover the cost of the leave.
What this means for employers?
- Employers may, but are not required to, continue providing paid leave that would have been required by the FFCRA from January 1, 2021 forward.
- Private-sector employers currently covered by the FFCRA who continue to provide paid leave can continue to claim a tax credit to cover the cost of voluntarily providing FFCRA leave through March 31, 2021.
- The amendment does not increase the total amount of the tax credit available to pay for leave for any single employee. FFCRA sick leave or expanded FMLA leave taken before December 31, 2020 will still count against the total amount of any tax credits that can be claimed for leave taken through March 31, 2021.
- Even though FFCRA leave will no longer be mandatory, employers must still comply with the ADA, FMLA, and leave mandates under state and local law.
- Employers with unionized workforces must also be mindful of contract and bargaining obligations related to any changes in their leave policies.
- Keep in mind that things could still change
- - - -
COVID-19 Grief Is Different: What Managers Should Know
By Kathleen Doheny
As COVID-19 cases and deaths continue to increase across the country, so do the number of workplaces dealing with employees' grief as their loved ones or co-workers become ill or die.
COVID-19 grief is different than other types of grief, warn mental health and grief experts. Managers can better help their workers cope if they understand some of these differences.
"COVID grief is disenfranchised grief," said psychiatrist Joshua Morganstein, chair of the American Psychiatric Association committee that issued special guidance for its members caring for patients affected by COVID-19 grief. "They are living with grief they are unable to express through normal outlets." Among the ways COVID-19 grief differs:
- Death from COVID-19 occurs quickly and randomly. Young, healthy people may die, while older people with medical issues recover.
- COVID-19's erratic nature—with some family members surviving and others not—can make survivor guilt worse than usual.
- The traditional goodbye to loved ones, with handholding and hugging, has sometimes been replaced by a cell phone conversation with a health care worker as the go-between.
- Social support for those grieving is often by e-mail, phone or Zoom, not in person.
- Other chaos, such as multiple loved ones falling sick or dying at the same time, fear of job loss, or financial problems can make the COVID-19 grieving process worse.
How can managers help? "We are not advocating that leaders become grief counselors," said Anthony Casablanca, a former HR executive who, with his brother Guy, a funeral director and mortician, co-founded GriefLeaders LLC, a training and consulting organization in the Indianapolis area that educates managers on how to help grieving employees. Rather, managers can reach out to see what the worker needs from them and from co-workers. Here's how.
Encourage workers to acknowledge the grief. Allow workers to talk about their grief, whether the deceased person or the COVID-19 patient is a co-worker, a boss or a family member, and join in the conversation, Morganstein said. For managers, "sometimes this is difficult," he said, as managers may worry, they will be perceived as losing control if they become emotional about others' grief. They may also worry they won't know how to handle things if a worker becomes overwhelmed by grief. "The manager can model that it's OK to be real," he said. A manager must be prepared to assume the role of a "grief leader."
When researching for their book on how to help grieving workers,The Dying Art of Leadership: How Leaders Can Help Grieving Employees(Bookbaby Publishing, 2020), Casablanca said workers often told him and his brother: "I was so thankful I could talk about my situation at work."
Suppress judgment. When someone first talks about a COVID-19 diagnosis, the judgment can be swift and overwhelming, said Rachel Kodanaz, a Denver consultant, grief expert, COVID-19 survivor and author ofGrief in the Workplace: A Comprehensive Guide to Being Prepared(GIW Publishing, 2015). "People often ask: 'Were you at a party?' or 'Did you wear a mask?' " Managers can remind their workers: As judgment increases, empathy decreases.
Keep quiet about your own story. Telling a grieving person your own grief experience might seem helpful, but it's not, Kodanaz said. It minimizes the feelings of the other person. At some point, she said, you might tell them you've had a grief experience and you're open to talking about it. But not when they are newly grieving. "This way they won't feel shut down."
Help workers find a way to honor those affected. This is important not only for workers who have experienced the death of a loved one or co-worker, Morganstein said, but also those who've experienced the sickness of a loved one or co-worker. For instance, if a co-worker is hospitalized with COVID-19 and was an avid runner, workers might decide to make a group video of themselves running and send it to the person or the person's loved ones, to show support and to show that they are thinking of them. The effort would likely help the group feel connected as well, Morganstein said, and that social connectiveness can ease grief.
Gauge the worker's immediate support need. "If an employee's spouse lost his job and they can't pay their bills, they may need more practical support than emotional," Morganstein said. For instance, a manager might consult with HR to see if there are discounts for necessities like childcare. "It's important that the managers not feel they have to do it all themselves," Morganstein said. They can lead the effort, but also rely on the help of other departments.
Be as flexible as possible. Bereavement benefits are often too brief, Casablanca said. About 88 percent of companies offer some paid bereavement leave, according to a 2018 Society of Human Resource Management survey. Most companies that offer the leave allow employees to take off two to four days for bereavement. To meet the need for longer time away, "we have found that managers have a lot of flexibility in adjusting work hours or allowing people to use vacation on short notice," Casablanca said. Before offering those possibilities, however, find out how the grieving worker is coping and what is needed.
Watch for signs of struggling. "Don't wait for performance to slip," Casablanca said. Be observant. If a generally talkative person clams up at meetings, that's the time to invite them to talk privately, Casablanca said. Instead of grilling them, simply let them know you are available to have a conversation about how things are going. Keep the talk simple and to the point; for example, say: "I can't imagine all the emotions you are feeling. We want to help you through this." Then, let them tell you how to do that.
- - - -
The Roles of Employers and Workers in Responding to COVID-19
The following information was updated on OSHA’s website on 1/29/21. Throughout this article are hyperlinks to information that can help your organization stay safe, in compliance, and assisting you in keeping your business moving forward during the pandemic.
Under the OSH Act, employers are responsible for providing a safe and healthy workplace free from recognized hazards likely to cause death or serious physical harm.
Implementing a workplace COVID-19 prevention program is the most effective way to mitigate the spread of COVID-19 at work.
The most effective COVID-19 prevention programs engage workers and their representatives in the program's development and implementation at every step, and include the following elements:
- Assignment of a workplace coordinator who will be responsible for COVID-19 issues on the employer's behalf.
- Identification of where and how workers might be exposed to COVID-19 at work. This includes a thorough hazard assessment to identify potential workplace hazards related to COVID-19. This assessment will be most effective if it involves workers (and their representatives) because they are often the people most familiar with the conditions they face.
-
Identification of a combination of measures that will limit the spread of COVID-19 in the workplace, in line with the principles of the hierarchy of controls. This should include a combination of eliminating the hazard, engineering controls, workplace administrative policies, personal protective equipment (PPE), and other measures, prioritizing controls from most to least effective, to protect workers from COVID-19 hazards. Key examples ([discussed in additional detail below] include:
In addition to these general guidelines, more specific guidance is available for certain industries.
- eliminating the hazard by separating and sending home infected or potentially infected people from the workplace
- implementing physical distancing in all communal work areas [includes remote work and telework];
- installing barriers where physical distancing cannot be maintained;
- suppressing the spread of the hazard using face coverings;
- improving ventilation;
- using applicable PPE to protect workers from exposure;
- providing the supplies necessary for good hygiene practices; and
- performing routine cleaning and disinfection.
- Consideration of protections for workers at higher risk for severe illness through supportive policies and practices. Older adults and people of any age who have serious underlying medical conditions are at higher risk for severe illness from COVID-19. Workers with disabilities may be legally entitled to "reasonable accommodations" that protect them from the risk of contracting COVID-19. Where feasible, employers should consider reasonable modifications for workers identified as high-risk who can do some or all of their work at home (part or full-time), or in less densely-occupied, better-ventilated alternate facilities or offices.
-
Establishment of a system for communicating effectively with workers and in a language they understand. Ask workers to report to the employer, without fear of reprisal (see 12 below), COVID-19 symptoms, possible COVID-19 exposures, and possible COVID-19 hazards at the workplace. Communicate to workers, in a language they can understand and, in a manner, accessible to individuals with disabilities, all policies and procedures implemented for responding to sick and exposed workers in the workplace. See below for additional elements involving educating and training workers of COVID-19 procedures.
In addition, a best practice is to create and test two-way communication systems that workers can use to self-report if they are sick or have been exposed, and that employers can use to notify workers of exposures and closures, respectively.
-
Educate and train workers on your COVID-19 policies and procedures using accessible formats and in a language they understand. Communicate supportive workplace policies clearly, frequently, in plain language that workers understand (including non-English languages, and American Sign Language or other accessible communication methods, if applicable), and in a manner accessible to individuals with disabilities, and via multiple methods to employees, contractors, and any other individuals on site, as appropriate, to promote a safe and healthy workplace. Communications should include:
- Basic facts about COVID-19, including how it is spread and the importance of physical distancing, use of face coverings, and hand hygiene. See About COVID-19 and What Workers Need to Know About COVID-19 above and see more on physical distancing, PPE, face coverings, and hygiene, respectively, below;
- Workplace policies and procedures implemented to protect workers from COVID-19 hazards (the employer's COVID-19 prevention program); and
- Some means of tracking which workers have been informed and when.
In addition, ensure that workers understand their rights to a safe and healthful work environment, whom to contact with questions or concerns about workplace safety and health, and their right to raise workplace safety and health concerns free of retaliation. This information should also be provided in a language that workers understand. (See Implementing Protections from Retaliation, below.) Ensure supervisors are familiar with workplace flexibilities and other human resources policies and procedures.
- Instruct workers who are infected or potentially infected to stay home and isolate or quarantine to prevent or reduce the risk of transmission of COVID-19. Ensure that absence policies are non-punitive. Policies that encourage workers to come to work sick or when they have been exposed to COVID-19 are disfavored. See below for additional guidance involving eliminating the hazard.
- Minimize the negative impact of quarantine and isolation on workers. When possible, allow them to telework, or work in an area isolated from others. If those are not possible, allow workers to use paid sick leave, if available, or consider implementing paid leave policies to reduce risk for everyone at the workplace. The Families First Coronavirus Response Act provides certain employers 100% reimbursement through tax credits to provide employees with paid sick leave or expanded family and medical leave for specified reasons related to COVID-19 through March 31, 2021.
- Isolating workers who show symptoms at work. Workers who appear to have symptoms upon arrival at work or who develop symptoms during their work shift should immediately be separated from other workers, customers, and visitors, sent home, and encouraged to seek medical attention. See below for additional elements involving screening and testing.
-
Performing enhanced cleaning and disinfection after people with suspected or confirmed COVID-19 have been in the facility. If someone who has been in the facility is suspected or confirmed to have COVID-19, follow the CDC cleaning and disinfection recommendations. This includes:
- Closing areas used by the potentially infected person for enhanced cleaning.
- Opening outside doors and windows to increase air circulation in the area.
- Waiting as long as practical before cleaning or disinfecting (24 hours is optimal).
- Cleaning and disinfecting all immediate work areas and equipment used by the potentially infected person, such as offices, bathrooms, shared tools and workplace items, tables or work surfaces, and shared electronic equipment like tablets, touch screens, keyboards, and remote controls.
- Vacuuming the space if needed. Use a vacuum equipped with a high-efficiency particulate air (HEPA) filter, if available. Wait until the room or space is unoccupied to vacuum.
- Providing cleaning workers with disposable gloves. Additional PPE (e.g., safety glasses, goggles, aprons) might be required based on the cleaning/disinfectant products being used and whether there is a risk of splash.
- After cleaning, disinfecting the surface with an appropriate EPA-registered disinfectant on List N: Disinfectants for use against SARS-CoV-2.
- Following requirements in OSHA standards 29 CFR 1910.1200 and 1910.132,133, and 138 for hazard communication and PPE appropriate for exposure to cleaning chemicals
Once the area has been appropriately disinfected, it can be opened for use. Workers without close contact with the potentially infected person can return to the area immediately after disinfection.
If it is more than 7 days since the infected person visited or used the facility, additional cleaning and disinfection is not necessary. Continue routine cleaning and disinfection, described below.
-
Providing guidance on screening and testing: Follow state or local guidance and priorities for screening and viral testing in workplaces. Testing in the workplace may be arranged through a company's occupational health provider or in consultation with the local or state health department. Employers should inform workers of employer testing requirements, if any, and availability of testing options. CDC has published strategies for consideration of incorporating viral testing for SARS-CoV-2, the virus that causes COVID-19, into workplace COVID-19 preparedness, response, and control plans. (See below for more on the use of testing to determine when a worker may return to work after illness or exposure)
Note: Performing screening or health checks is not a replacement for other protective measures such as face coverings and physical distancing. Asymptomatic individuals or individuals with mild non-specific symptoms may not realize they are infected and may not be detected during through screening.
-
Recording and reporting COVID-19 infections and deaths: Employers are responsible for recording work-related cases of COVID-19 illness on their Form 300 logs if the following requirements are met: (1) the case is a confirmed case of COVID-19; (2) the case is work-related (as defined by 29 CFR 1904.5); and (3) the case involves one or more relevant recording criteria (set forth in 29 CFR 1904.7) (e.g., medical treatment, days away from work). Employers must follow the requirements in 29 CFR 1904 when reporting COVID-19 fatalities and hospitalizations to OSHA. More information is available on OSHA's website. Employers should also report outbreaks to health departments as required and support their contact tracing efforts.
In addition, employers should be aware that reprisal or discrimination against an employee for speaking out about unsafe working conditions or reporting an infection or exposure to COVID-19 to an employer or OSHA would constitute a violation of Section 11(c) of the Act. In addition, 29 CFR 1904.35(b) also prohibits discrimination against an employee for reporting a work-related illness.
-
Implementing protections from retaliation and setting up an anonymous process for workers to voice concerns about COVID-19-related hazards: Section 11(c) of the OSH Act prohibits discharging or in any other way discriminating against an employee for engaging in various occupational safety and health activities. For example, employers may not discriminate against employees for raising a reasonable concern about infection control related to COVID-19 to the employer, the employer's agent, other employees, a government agency, or to the public, such as through print, online, social, or any other media; or against an employee for voluntarily providing and wearing their own personal protective equipment, such as a respirator, face shield, gloves, or surgical mask.
In addition to notifying workers of their rights to a safe and healthful work environment, ensure that workers know whom to contact with questions or concerns about workplace safety and health, and that there are prohibitions against retaliation for raising workplace safety and health concerns or engaging in other protected occupational safety and health activities (see educating and training workers about COVID-19 policies and procedures, above); also consider using a hotline or other method for workers to voice concerns anonymously.
- Making a COVID-19 vaccine or vaccination series available at no cost to all eligible employees. Provide information and training on the benefits and safety of vaccinations.
- Not distinguishing between workers who are vaccinated and those who are not: Workers who are vaccinated must continue to follow protective measures, such as wearing a face covering and remaining physically distant, because at this time, there is no evidence that COVID-19 vaccines prevent transmission of the virus from person-to-person. The CDC explains that experts need to understand more about the protection that COVID-19 vaccines provide before deciding to change recommendations on steps everyone should take to slow the spread of the virus that causes COVID-19.
- Other applicable OSHA Standards All of OSHA's standards that apply to protecting workers from infection remain in place. These standards include: requirements for PPE (29 CFR 1910, Subpart I (e.g.,[1910.132 and 133)), respiratory protection (29 CFR 1910.134), sanitation (29 CFR 1910.141), protection from bloodborne pathogens: (29 CFR 1910.1030), and OSHA's requirements for employee access to medical and exposure records (29 CFR 1910.1020). There is no OSHA standard specific to COVID-19; however, employers still are required under the General Duty Clause,[Section 5(a)(1) of the OSH Act, to provide a safe and healthful workplace that is free from recognized hazards that can cause serious physical harm or death.
Other areas that employers should be evaluating and additional information on this topic can be found at: https://www.osha.gov/coronavirus/safework
- - - -
Contact HR Strategies staff at 302.376.8595 or info@hrstrategies.org if you would like support or would like to learn more about the items in this newsletter. Please contact us if you would like to be added to our Monthly Strategies mailing list or if you would like for us to add someone to our mailing list.